Do Cholesterol-lowering Statin Drugs Really Work? Who Benefits? Who Has the Power to Cover Up the Side Effects?
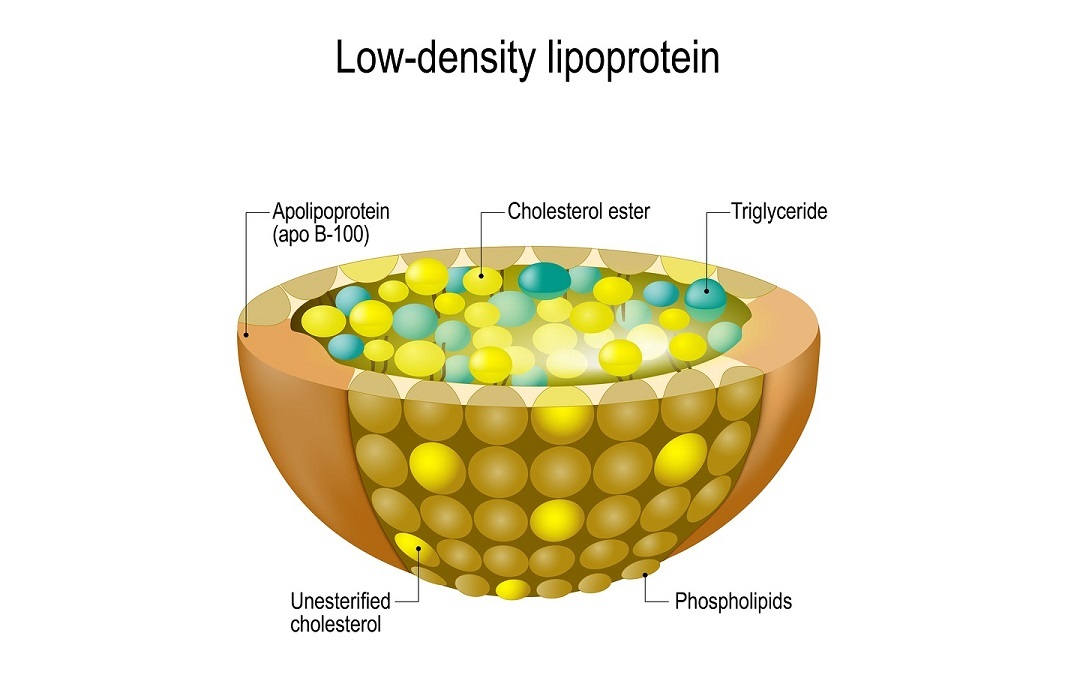
For decades, the medical establishment in the U.S., Canada, and the UK has promoted statin drugs for an ever increasing population. Concomitantly, public health officials have advocated a low fat high carbohydrate diet, and the replacement of saturated fat with polyunsaturated fats. By following this regimen, the medical “authorities” claimed, will prevent heart disease. Nobel Prize winners Dr. Michael Brown and Dr. Joseph Goldstein who discovered the central role that blood cholesterol played in the development of heart disease, prompted the pharmaceutical industry to develop statins. Although the scientists’ prediction that heart disease will have disappeared by the beginning of the 21st century, was decidedly wrong, the manufacturers of statins have profited beyond expectations – even though the drugs have not reduced heart disease. Like so many flawed, but widely recommended medical regimens, this one is not about improving public health. Independent physicians who are not industry lackeys agree that cardiovascular disease are likely to be preventable through modifying the diet by lower sugar and carbohydrates, increased exercise, and eliminating tobacco use. But healthy lifestyle regimens don’t generate billions of dollars!