The Healing Oils for Heart Health: Do NOT Trust Your Government for Nutritional Advice
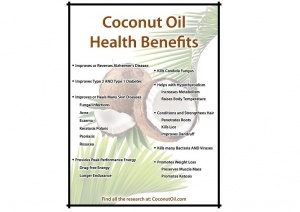
As more and more people in the United States are waking up to the fact that our federal health agencies, such as the FDA and CDC, are corrupt and serve the interests of Wall Street Billionaires and not the public, it is more important than ever to understand the corruption that also exists within the USDA (U.S. Department of Agriculture) and their years of bad nutritional advice that has demonized traditional, healthy fats and oils that have nourished populations for thousands of years, in favor of the newer "polyunsaturated" oils which are toxic, and dangerous to your health. These polyunsaturated "edible oils" have only been in the human food chain since the "expeller-pressed" technology was developed during and following World War II that allowed the U.S. to start producing highly toxic and refined "edible" oils from corn and soybeans, two crops heavily subsidized by taxpayers that allows the U.S. to dominate world edible oil supplies. It was in the 1970s that the "McGovern Report" put forward the nutritional dietary advice of a "low-fat" diet that harmed American's health by condemning traditional fats and oils, but brought great profit to Wall Street investors as Americans switched over to hydrogenated toxic polyunsaturated oils derived from corn and soybeans. They used a theory of heart disease commonly referred to as the "lipid theory" of heart disease that stated certain kind of fats, saturated fats, led to higher levels of cholesterol, and therefore higher risks for heart disease. But even from the beginning and the origin of this theory what was stated in the McGovern Report, many scientists disagreed and called the theory bogus. Today, the lipid theory of heart disease has been thoroughly debunked by real science, and yet official government policy on nutrition continues to support it, for political and economic reasons, but NOT health reasons. To admit that they were wrong all these years on dietary oils, cholesterol, and heart disease, would be to admit that the $BILLIONS they earned during that time from popular cholesterol-lowering drugs, was earned fraudulently, and the biggest player in that industry was Pfizer, and their blockbuster drug Lipitor, the best-selling drug all-time before its patent ran out in 2011. So with Pfizer's newest killer drug, the COVID-19 vaccine, injuring the hearts of many people with myocarditis and pericarditis, especially among the younger age groups, it is more important than ever to understand just which dietary oils are actually healthy for the heart, and which ones are not.